Background
Patients with acute lymphoblastic leukemia (ALL) are at increased risk of thrombotic and or bleeding events during chemotherapy, especially when receiving L-Asparaginase (ASP). Previous studies have identified variables associated with increased thrombotic risk in ALL including age, body mass index (BMI), sex, platelet count, and ASP use (Orvain 2020); however, to date no ALL-based study has examined D-dimer, a marker of fibrinolysis that has been shown to predict thrombosis in acute myelogenous leukemia (AML) (Libourel 2016), in this context. We sought to examine the utility of D-dimer as a biomarker for risk of thrombosis or bleeding events during ALL treatment.
Methods
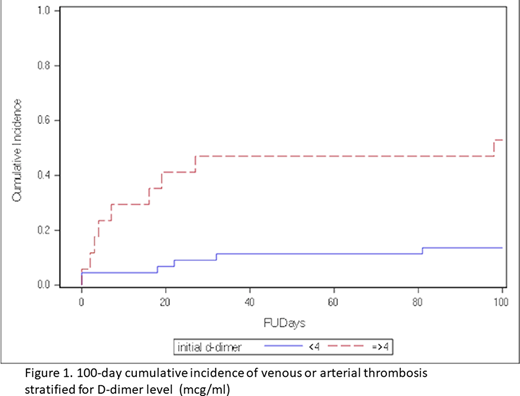
In this retrospective cohort study we identified 61 adult patients with newly diagnosed ALL from a single center between 2008 and 2020. Patient demographic details, treatment regimens, and biomarkers including D-dimer (ordered routinely at diagnosis as a serum assay in mcg/ml FEU) were ascertained. Patients were stratified according to D-dimer level using a cut-off of ≥4 mcg/ml (high) and <4 mcg/ml (low-moderate) based upon previous work examining D-dimer and thrombosis in AML (Libourel 2016). The disseminated intravascular coagulation (DIC) score according to the International Society on Thrombosis and Haemostasis (ISTH) was calculated at diagnosis. Major and clinically relevant non-major bleeding and first arterial or venous thrombotic event (confirmed by imaging) within 100 days of ALL diagnosis were recorded. The 100-day cumulative incidence of thrombosis was calculated for both D-dimer groups. Event rate was compared between D-dimer groups using chi-square analysis. Logistic regression was used to examine D-dimer as a continuous or categorical variable and compare events through 100 days. Six multivariate models, each including D-dimer and one of six previously identified thrombosis risk factors were performed. A receiver operating characteristic curve (ROC) was generated and area under the curve (AUC) calculated.
Results
Sixty-one patients with ALL were included; 52% were female and 48% male. Median age was 36 years (range 18-84). Patients were 18% Black, 26% Latinx, 52% White, and 3.3% Asian/Mideast Indian. Immunophenotypes included B-cell (82%), T-cell (8.2%), and mixed phenotype ALL (9.8%), with 24% of patients having Ph + or Ph-like status. ASP-based regimens were utilized in 67% of patients.
The median D-dimer level was 2.1 mcg/ml (range: 0.26 to 20). The 100-day cumulative incidence of thrombosis was 53% (95% CI 26.4-73.8) in the high D-dimer group (N=17, 28%) and 14% (95% CI 5.5 - 25.5) in the low-moderate D-dimer group (N=44, 72%) (Figure 1). The rate of thrombosis was higher in the high D-dimer group, X2 (1, N=61) =10.2, p=.001. The odds of thrombosis within 100 days increased by 1.65 per every 3-unit increase in D-dimer (95% CI 1.2-2.27). The association between D-dimer and thrombosis remained after including additional confounders such as BMI, age, sex, ASP status, DIC score, and initial platelet level in covariate logistic regression models. ROC analysis demonstrated 60% sensitivity and 80% specificity for a D-dimer cutoff of 4 mcg/ml, with an AUC of 0.798 (95% CI 0.67-0.92). Clinically relevant bleeding occurred in 8 patients (13%) during the first 100 days after diagnosis and was not significantly associated with initial D-dimer level, BMI, age, sex, ASP status, DIC score, or initial platelet level.
Conclusion
High D-dimer (≥4 mcg/ml) at ALL diagnosis is associated with an increased rate of venous or arterial thrombosis within the first 100 days, with no increased rate of clinically relevant bleeding. D-dimer as a continuous variable appears to have good independent diagnostic discrimination for thrombosis. Prospective studies aiming to create ALL-specific thrombosis risk assessment models are warranted and should consider D-dimer level at diagnosis together with previously identified risk factors (Al-Ani 2020, Orvain 2020).
Leader:Bayer Healthcare: Other: personal fees ; Pfizer Pharmaceuticals Israel Ltd.: Consultancy, Honoraria, Other: personal fees .
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal